TEL: (818) 907-7828 | EMAIL: sharon@statmedical.net
What Does Revenue Cycle Management Mean?
Unearth Every Aspect of Revenue Cycle Management
Revenue Cycle Management (RCM) serves as the financial backbone for healthcare facilities, utilizing advanced medical billing software to navigate the entire patient care journey, from initial registration and appointment scheduling to the ultimate balance payment. While finance is a vital aspect of every industry, the processes to manage are also different for each industry. Similarly, the name for the whole process that is adopted to manage finances varies as well. Revenue Cycle Management is specifically related to the healthcare industry. It refers to the process from patient registration to payment and is termed Revenue Cycle Management. RCM seamlessly integrates both the business and clinical aspects of healthcare by linking administrative data, including patient details and insurance information, with the specific treatment and healthcare data a patient receives.
A critical facet of revenue cycle management involves constant communication with health insurance companies. Before a scheduled appointment, healthcare providers verify a patient's reported insurance coverage. Following treatment, the provider or coder classifies the nature of the care using ICD-10 codes. The facility then forwards the care summary with codes to the patient's insurance company to determine coverage, with the patient responsible for any remaining balance.
Revenue Cycle Detail
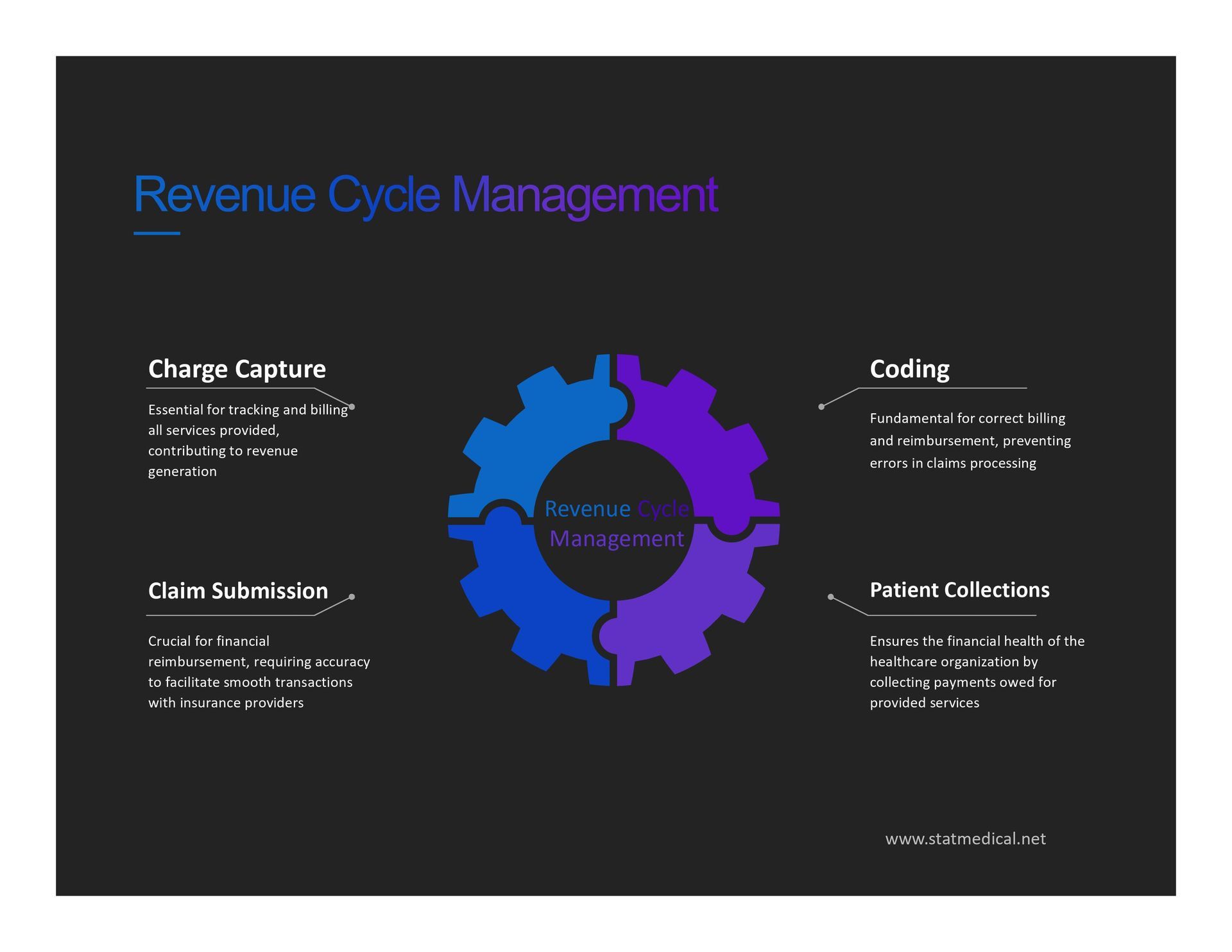
The comprehensive revenue cycle encompasses all administrative and clinical functions essential for capturing, managing, and collecting patient service revenue, as outlined by the Healthcare Financial Management Association (HFMA). Key components include charge capture, claim submission, coding, patient collections, preregistration, registration, remittance processing, third-party follow-up, and utilization review, collectively ensuring a streamlined and efficient financial process in healthcare operations.
Charge Capture:
Involves translating medical services into billable charges. It ensures that all provided services are accurately documented for billing purposes.
Claim Submission:
The process of submitting claims of billable fees to insurance companies for reimbursement. It involves providing detailed information about the services rendered.
Coding:
Properly coding diagnoses and procedures according to standardized code systems (e.g., ICD-10 codes). Accurate coding is crucial for correct billing and reimbursement.
Patient Collections:
Involves determining patient balances and collecting payments for services rendered. This component ensures the financial responsibility of patients is addressed.
Preregistration:
Collecting essential information, such as insurance coverage, before a patient arrives for inpatient or outpatient procedures. It streamlines the registration process.
Registration:
Involves collecting additional patient information during registration to establish a medical record number and meet regulatory, financial, and clinical requirements.
Remittance Processing:
Refers to applying or rejecting payments received through remittance processing. It ensures accurate recording of payments and facilitates reconciliation.
Third-Party Follow-Up:
Involves collecting payments from third-party insurers. This component ensures that all avenues for reimbursement are explored and addressed.
Utilization Review:
Examining the necessity of medical services provided. It involves evaluating the appropriateness and efficiency of healthcare resources utilized during patient care.
Other Factors Influencing the Revenue Cycle
Various factors influence the revenue cycle in healthcare, encompassing both internal and external dynamics. Internal factors, including provider productivity, patient volume, and service fees, fall within the healthcare organization's control. Conversely, external factors like patient payments and insurance claim reviews pose challenges that are more difficult to manage.
Revenue Cycle Management Systems
To streamline revenue-related processes, healthcare providers often adopt specialized Revenue Cycle Management (RCM) systems. These systems, integrated with electronic health records (EHR) and medical billing systems, enhance efficiency by reducing the time between service provision and payment receipt. Revenue cycle management systems automate tasks, such as appointment reminders and balance notifications, previously handled by staff, resulting in time and cost savings.
These systems also play a pivotal role in addressing denied claims. By prompting thorough information entry for claims processing, revenue cycle management systems minimize the need for claim revisions or resubmissions, providing valuable insights into denial reasons. This ensures accurate reimbursement for services rendered to Medicare patients.
Data analytics and dashboards further aid organizations in setting and monitoring revenue goals. RCM systems, incorporating technologies like cognitive computing and robotic process automation, contribute to accurate medical coding and process acceleration.
As the healthcare industry shifts towards value-based care, revenue cycle management systems play a crucial role. They facilitate detailed analytics on patient populations and claims data, aligning with initiatives like the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) promoting value-based reimbursement.
Major vendors in the revenue cycle management space, offering standalone products or integrated systems with EHR, include McKesson, Cerner, GE Healthcare, ADP, Epic Systems, Allscripts, Athenahealth, Dell EMC, Greenway Health, and Meditech. The Healthcare Financial Management Association (HFMA) also plays a significant role, in advocating for finance professionals and promoting standards in healthcare finance.
Conclusion
In conclusion, navigating the complexities of revenue cycle management is paramount for sustained success in the healthcare industry. With over 30 years of expertise, Stat Medical Consulting, Inc. stands out as a premier billing company, offering unparalleled insights and solutions. Entrust your financial health to a consultancy that understands the intricacies of the field, ensuring optimal results for your organization.
-
What is the primary objective of Revenue Cycle Management?
The primary objective of Revenue Cycle Management is to ensure precise financial transactions at every stage. This involves identifying and rectifying any weaknesses in the monetary flow to maintain a seamless and accurate process.
-
What are the reasons for healthcare facilities to utilize RCM software solutions?
Medical RCM software streamlines tasks in healthcare facilities, ensuring accurate scheduling, billing, and coding for efficient claim processing and payment collection. This electronic solution enhances accuracy, efficiency, and allows the team to focus on high-priority responsibilities.
-
What factors should be considered when choosing an RCM system?
When healthcare organizations choose an RCM system, it's crucial to ensure the system offers versatile and customizable applications, allowing each organization to tailor the system to its specific requirements. Key features to seek include efficient patient registration, seamless collections, and provider-friendly charting.
-
How can you determine the effectiveness of your RCM performance?
Assessing the performance of your RCM involves analyzing key benchmarks such as copayment collections, days in accounts receivable, days in total discharged not billed, clean claim rate, and bad debt. These metrics provide insights into the efficiency and effectiveness of your revenue cycle management, guiding improvements where needed.
-
What makes healthcare revenue cycle management intricate?
The complexity arises from managing rising costs, preventing unpaid claims, optimizing point-of-service collections, and enhancing coding and billing processes to sustain profit margins.

Address:
Stat Medical Consulting, Inc
22801 Ventura Boulevard, Suite 211, Woodland Hills, CA 91364
Email: sharon@statmedical.net
Phone:
818-907-7828

Stat Medical Consulting, Inc